by Patrick Kuhn | Aug 28, 2025 | Media Post
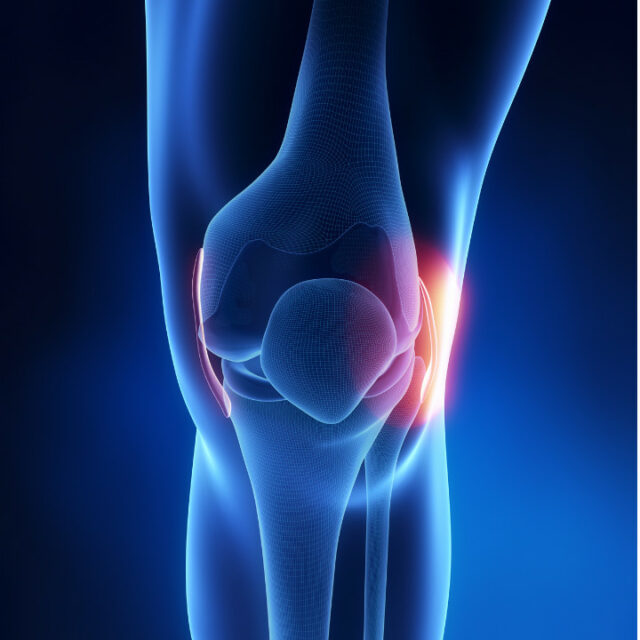
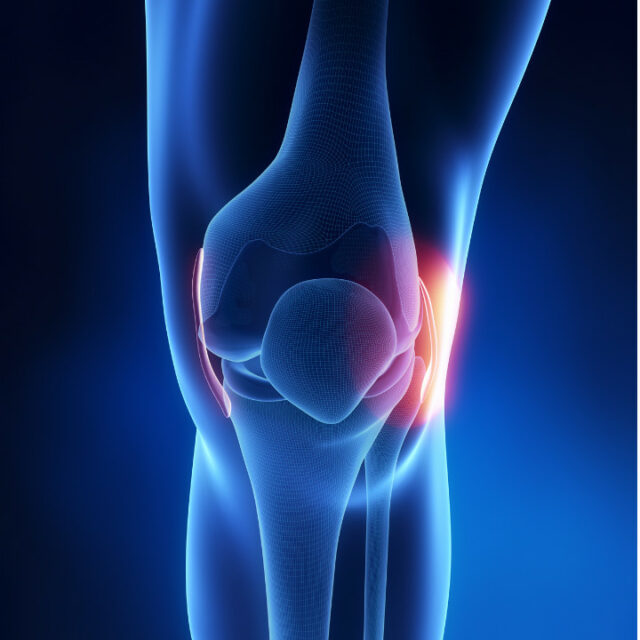
MCL Injuries
The Medial Collateral Ligament (MCL) is one of the key stabilisers of your knee. Running along the inside of the joint, it prevents the knee from collapsing inwards during movement. Because of its role, the MCL is commonly injured in sports and activities that involve twisting, sudden changes in direction, or direct impact.
What causes MCL injuries?
MCL injuries usually occur when a force is applied to the outside of the knee, causing the joint to bend inward. This is particularly common in sports like soccer, football, and skiing, where collisions, awkward landings, or sharp turns put the knee under extra stress.
They can also happen from degenerative causes, where tears in the ligament can slowly develop over time due to repetitive stress and natural wear and tear on the knee.
Common symptoms of an MCL injury:
- Localised pain or tenderness on the inner side of the knee
- Swelling or stiffness along the joint line
- A feeling of instability in the knee
- Difficulty weight-bearing or changing direction
Why early assessment matters
Many people try to “walk off” a knee injury, but ignoring pain can delay healing or increase the risk of further damage. Early assessment ensures that the injury is properly diagnosed, and a tailored rehabilitation plan can be put in place.
How we can help
Our osteopaths provide hands-on treatment to reduce pain and swelling, improve mobility, and restore proper movement patterns. We’ll guide you through a structured rehab program to help strengthen and stabilise your knee, so you can return to sport or daily activities with confidence.
If you’ve injured your knee or are experiencing inner knee pain, don’t wait it out – getting the right care early makes all the difference.
If you have questions about MCL strains and how our osteopaths might be able to help, please call us on 03 5968 6889 or email info@emeraldosteopathy.com.au. We would love to work with you!
Copyright 2023 Emerald Osteopathy Sports & Spinal | All Rights Reserved | Abn 28 134 053 633 | Sitemap | web : footprintweb.com.au | MyDash

by Patrick Kuhn | Jul 30, 2025 | Media Post
Ligament Sprains
Ligament Sprains – What they are and tips to prevent them
Rolled your ankle or twisted your knee? You might be dealing with a ligament sprain – an injury where the bands that stabilise your joints get overstretched or torn.
Why do sprains happen?
- Sudden twists, falls, or awkward landings
- Poor warm-up or muscle fatigue
- Unstable surfaces or improper footwear
Common signs include:
- Swelling
- Bruising
- Pain when moving or bearing weight
- Feeling of instability
Tips to prevent sprains:
- Strengthen muscles around your joints
- Improve balance and proprioception
- Warm up properly before activity
- Wear supportive footwear
If you’ve had a sprain before, you’re more likely to get another—so early rehab and proper recovery are key.
Feeling unstable or sore? Let us help you get back on track with the right treatment and movement advice.
If you have questions about Ligament Sprains and how our osteopaths might be able to help, please call us on 03 5968 6889 or email info@emeraldosteopathy.com.au. We would love to work with you!
Copyright 2023 Emerald Osteopathy Sports & Spinal | All Rights Reserved | Abn 28 134 053 633 | Sitemap | web : footprintweb.com.au | MyDash

by Patrick Kuhn | Jul 24, 2025 | Media Post
Muscle Strains:
Why They Happen & How to Prevent Them
Muscle strains – those sudden pulls or tears – are common in both athletes and weekend
warriors. They often happen when a muscle is overloaded or overstretched.
Common causes include:
Skipping warm-ups
Poor movement mechanics
Muscle fatigue or weakness
Overtraining
Sudden bursts of movement such as sprinting or lifting too heavy too soon
Prevent muscle strains with these tips:
Warm up with dynamic movement
Build strength gradually
Include flexibility & mobility work
Rest and recover between sessions
Pay attention to technique
Feeling tight, sore, or unsure if you’ve strained something? Our osteopaths are here to help!
To make an appointment book online at emeraldosteopathy.com.au or call us at 03 5968
6889 today!
Copyright 2023 Emerald Osteopathy Sports & Spinal | All Rights Reserved | Abn 28 134 053 633 | Sitemap | web : footprintweb.com.au | MyDash

by Patrick Kuhn | May 22, 2025 | News Letter
L5-S1 Disc Bulge Injury

What is a disc injury?
Disc injuries refer to damage or dysfunction of the intervertebral discs, which are the soft, cushion-like pads between the bones (vertebrae) of your spine. These discs act as shock absorbers and allow flexibility in your back. Disc injuries are common, especially in the lumbar spine (lower back).
L5/S1 disc injuries affect the disc located between the 5th lumbar vertebra (L5) and the 1st sacral vertebra (S1) – the junction between the spine and pelvis. This area is a common site for disc herniation and degeneration because it bears significant weight and endures a lot of mechanical stress, especially during bending and lifting.
What causes disc injuries?
Disc injuries can be categorized into two main causes:
- Degeneration – normal age-related wear and tear to the disc
- Mechanical/Traumatic causes, which can include:
- Heavy lifting or repetitive bending, especially with poor technique
- Sudden trauma or impact – falls, car accidents, sports injuries
- Prolonged sitting or poor posture
- Overuse and repetitive stress – jobs involving heavy physical labor, heavy weightlifting etc.
Other risk factors:
- Obesity
- Poor core strength
- Family history/Genetic predisposition
What are the symptoms of L5/S1 disc injuries?
- Lower back pain at the base of the spine
- Sciatic pain (sharp or burning pain down the buttock, leg and foot)
- Numbness and tingling in the back of the leg and foot
- Weakness in the leg and foot
How can osteopathy help?
Our Osteopaths can help with the management of disc injuries in multiple ways, including:
- Assessment and diagnosis of your condition
- Manual therapy to relieve pain and improve mobility
- Exercise prescription to improve strength and muscle imbalances that may be contributing to your pain
- Education and advice on pain management and lifestyle modification to help manage your condition
If you have questions about disc injuries and how our osteopaths might be able to help, please call us on 03 5968 6889 or email info@emeraldosteopathy.com.au. We would love to work with you!
Omega-3’s Effect and Benefits

Omega-3 fatty acids—especially EPA (eicosapentaenoic acid) and DHA (docosahexaenoic acid)—can offer several benefits for connective tissue health, including joints, tendons, ligaments, and fascia. Here’s a breakdown of how omega-3s support connective tissue:
Benefits of Omega-3 for Connective Tissue
🦴 1. Anti-Inflammatory Effects
-
Omega-3s reduce the production of inflammatory cytokines and prostaglandins.
-
This helps decrease chronic inflammation that damages connective tissue over time (common in arthritis, tendonitis, etc.).
💪 2. Improved Collagen Formation
-
Some research suggests omega-3s can support collagen synthesis by reducing oxidative stress and inflammation, both of which degrade collagen.
-
Collagen is the main structural protein in connective tissue.
🧠 3. Reduction in Joint Pain and Stiffness
🔧 4. Protection Against Connective Tissue Breakdown
🏃 5. Enhanced Tendon and Ligament Healing
Sources of Omega-3s
-
Fatty fish (salmon, sardines, mackerel, herring)
-
Fish oil supplements
-
Algal oil (vegan source of DHA)
-
Flaxseed, chia seeds, walnuts (contain ALA, which converts inefficiently to EPA/DHA)
Recommended Intake
-
General health: 250–500 mg of EPA + DHA daily.
-
For inflammation/pain relief: 1,000–3,000 mg daily (split into 2–3 doses, ideally with food).
-
Always check with a healthcare provider if you’re on blood thinners or have a bleeding disorder.
One-Pot Garlicky Shrimp & Broccoli
 This One-Pot Garlicky Shrimp & Broccoli dish will have dinner on the table lickety-split—perfect for busy weeknights. Antioxidant-rich broccoli and red bell pepper become fork-tender and toothsome without becoming mushy. Protein-filled shrimp bring a taste of the sea, while garlic adds its classic spiciness. A touch of lemon at the end adds a light, bright finish. Plus, it’s gluten-free. Keep reading for our expert tips, including what to serve with this dish.
This One-Pot Garlicky Shrimp & Broccoli dish will have dinner on the table lickety-split—perfect for busy weeknights. Antioxidant-rich broccoli and red bell pepper become fork-tender and toothsome without becoming mushy. Protein-filled shrimp bring a taste of the sea, while garlic adds its classic spiciness. A touch of lemon at the end adds a light, bright finish. Plus, it’s gluten-free. Keep reading for our expert tips, including what to serve with this dish.
Nutrition Notes
- Broccoli is a fiber-filled, antioxidant-rich cruciferous vegetable that is loaded with health benefits. Eating more cruciferous veggies, like broccoli, may reduce your risk of cancer and heart disease, improve gut health and bolster your immune system. The red bell pepper adds more of these same benefits, since both vegetables reduce inflammation throughout the body.
- Shrimp is an excellent source of muscle-building lean protein. While shrimp is high in cholesterol, the cholesterol in the food we eat has little impact on our blood cholesterol. What does impact our bodies’ cholesterol levels is saturated and trans fats. Since shrimp has virtually none of either, it is considered a healthy source of protein—plus other essential nutrients, including heart-healthy omega-3s.
- Garlic has been linked with numerous health benefits, including a healthier heart, immune system, gut and blood sugar levels. While you probably eat only a small amount of garlic now and then, its potential health benefits are more likely to add up and have an impact by increasing how frequently you eat it.
Ingredients
- 3 tablespoons extra-virgin olive oil, divided
- 6 medium cloves garlic, sliced, divided
- 4 cups small broccoli florets
- ½ cup diced red bell pepper
- ½ teaspoon salt, divided
- ½ teaspoon ground pepper, divided
- 1 pound peeled and deveined raw shrimp (21-30 count)
- 2 teaspoons lemon juice, plus more to taste
Directions
-
Heat 2 tablespoons oil in a large pot over medium heat. Add half the garlic and cook until beginning to brown, about 1 minute. Add 4 cups broccoli, 1/2 cup bell pepper and 1/4 teaspoon each salt and pepper. Cover and cook, stirring once or twice and adding 1 tablespoon water if the pot is too dry, until the vegetables are tender, 3 to 5 minutes. Transfer to a bowl and keep warm.
- Increase heat to medium-high and add the remaining 1 tablespoon oil to the pot. Add the remaining garlic and cook until beginning to brown, about 1 minute. Add 1 pound of shrimp and the remaining 1/4 teaspoon each salt and pepper; cook, stirring, until the shrimp are just cooked through, 3 to 5 minutes. Return the broccoli mixture to the pot along with 2 teaspoons lemon juice and stir to combine.
Copyright 2023 Emerald Osteopathy Sports & Spinal | All Rights Reserved | Abn 28 134 053 633 | Sitemap | web : footprintweb.com.au | MyDash

by Patrick Kuhn | May 13, 2025 | Media Post
 L5-S1 Disc Bulge Injury
L5-S1 Disc Bulge Injury
What is a disc injury?
Disc injuries refer to damage or dysfunction of the intervertebral discs, which are the soft, cushion-like pads between the bones (vertebrae) of your spine. These discs act as shock absorbers and allow flexibility in your back. Disc injuries are common, especially in the lumbar spine (lower back).
L5/S1 disc injuries affect the disc located between the 5th lumbar vertebra (L5) and the 1st sacral vertebra (S1) – the junction between the spine and pelvis. This area is a common site for disc herniation and degeneration because it bears significant weight and endures a lot of mechanical stress, especially during bending and lifting.
What causes disc injuries?
Disc injuries can be categorized into two main causes:
- Degeneration – normal age-related wear and tear to the disc
- Mechanical/Traumatic causes, which can include:
- Heavy lifting or repetitive bending, especially with poor technique
- Sudden trauma or impact – falls, car accidents, sports injuries
- Prolonged sitting or poor posture
- Overuse and repetitive stress – jobs involving heavy physical labor, heavy weightlifting etc.
Other risk factors:
- Obesity
- Poor core strength
- Family history/Genetic predisposition
What are the symptoms of L5/S1 disc injuries?
- Lower back pain at the base of the spine
- Sciatic pain (sharp or burning pain down the buttock, leg and foot)
- Numbness and tingling in the back of the leg and foot
- Weakness in the leg and foot
How can osteopathy help?
Our Osteopaths can help with the management of disc injuries in multiple ways, including:
- Assessment and diagnosis of your condition
- Manual therapy to relieve pain and improve mobility
- Exercise prescription to improve strength and muscle imbalances that may be contributing to your pain
- Education and advice on pain management and lifestyle modification to help manage your condition
If you have questions about disc injuries and how our osteopaths might be able to help, please call us on 03 5968 6889 or email info@emeraldosteopathy.com.au. We would love to work with you!
Copyright 2023 Emerald Osteopathy Sports & Spinal | All Rights Reserved | Abn 28 134 053 633 | Sitemap | web : footprintweb.com.au | MyDash






 This One-Pot Garlicky Shrimp & Broccoli dish will have dinner on the table lickety-split—perfect for busy weeknights. Antioxidant-rich broccoli and red bell pepper become fork-tender and toothsome without becoming mushy. Protein-filled shrimp bring a taste of the sea, while garlic adds its classic spiciness. A touch of lemon at the end adds a light, bright finish. Plus, it’s gluten-free. Keep reading for our expert tips, including what to serve with this dish.
This One-Pot Garlicky Shrimp & Broccoli dish will have dinner on the table lickety-split—perfect for busy weeknights. Antioxidant-rich broccoli and red bell pepper become fork-tender and toothsome without becoming mushy. Protein-filled shrimp bring a taste of the sea, while garlic adds its classic spiciness. A touch of lemon at the end adds a light, bright finish. Plus, it’s gluten-free. Keep reading for our expert tips, including what to serve with this dish.